In Part 1 of our blog on Heart Health and Wellness, we looked at some very basic information about the heart. We learned about the spectrum of its functions on physical, mental/emotional, and spiritual realms of an individual person. We took a brief look at the overwhelming numbers of heart disease-related illness and deaths and highlighted some blind spots of drug interventions like statins.
Here in Part 2 of our discussion, we’ll take a deeper dive into Ayurvedic and Naturopathic understanding of the cardiovascular function as well as diseases and their treatments through natural means like diet, daily routines, and herbal medicines. For sake of simplification, we will only focus on the physical heart and cardiovascular treatments.
The heart and primitive circulatory system begins function in the fetus as early as 5 weeks after conception. From this point, to then end of its life, the heart beats and circulates blood, plasma, nutrition, and hormone to all parts of the body. The physical susceptibility of the heart also comes from this function. The circulatory system is the major superhighway that facilitates the body’s energy exchange and internal detoxification. For this reason, it’s the place where all travelers of the blood stream interact; these travelers include nutrition from our food, blood cells, immune cells, hormonal signals, platelets, and toxicants that are released by various cells back into the bloodstream. This role of the circulatory system makes it a very dramatic place and very vulnerable place for developing disease.
Major Causes of Heart Disease
As the leading cause of chronic illness and death in the United States, heart disease and its prevalence is an important reflection of the American health culture. The three major risk factors of heart disease are high blood pressure, elevated low-density lipoproteins (LDL) cholesterol, and smoking. About 49% of Americans have at least one of these three risk factors.1 Among these, high blood pressure is the most common risk factor of heart disease, most likely because blood pressure can be affected by physiological and psychological factors.
Additionally, the CDC points out other factors that might raise the risk of heart disease. Health conditions include high blood pressure, diabetes, elevated LDL cholesterol, and being overweight or obese. Lifestyle choices include smoking, poor diet, physical inactivity, and excessive alcohol use.
Ayurvedic philosophy divides the causes of imbalance into three categories:
Excess—Diabetes, obesity, smoking, excessive alcohol use
Deficiency—Poor diet associated with nutritional deficiencies, physical inactivity
Unhealthy combinations—Stress combined with unhealthy coping techniques, eating at in-correct times and quantities, eating combinations of fatty food and inflammatory foods, and lack of knowledge and complacency
To deal with the burden on the heart, we must develop the most efficient corrective approach that’s based on an individual’s lifestyle choices, disease risk factors, family history, and day-to-day circumstances that cause physical and emotional stress. This is holistic medicine, and it’s more powerful than pills. In fact, there are no pills that understand a person and his or her life. If your doctor is not taking the time to understand you and your life, it is assured that you are not being treated to the fullest extent of your capacity to heal. For this reason, many become dependent on pills for the rest of their lives.
Plaque in the Arteries
Most people interested in heart health are familiar with plaque in the arteries. We’ve seen the advertisements of statins, which show a drug breaking up the plaque to open up blood vessels. One this is clear: These are false advertisements. Statins only help to reduce cholesterol in the body, but do not have any role in breaking up plaque.
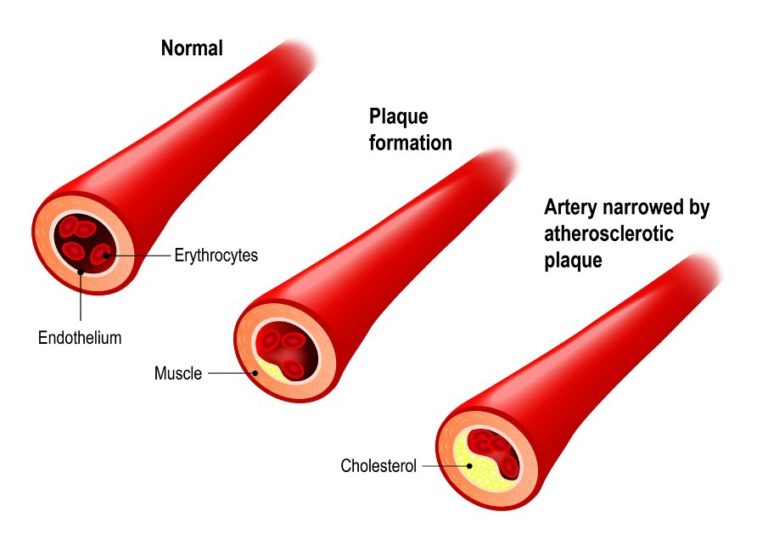
Plaque in the blood vessels is a combination of cholesterol fat, inflammation, immune cells, calcium deposits, and platelets.2This topic is very detailed and complex, and we couldn’t possibly address it all in one or two blog articles. However, the important part is that plaque is created when inflammation causes cholesterol—especially large molecules of fat, like LDL—to become oxidized and stuck on the blood vessel wall. Here, it becomes an obstruction in the blood flow and invites more inflammation and platelets to follow. In the end, we’re left with a microscopic scab on our blood vessel wall that has layers of fat, inflammatory cells, connective tissue, and calcium. Imagine a rough patch of cement plastered over a bump in the road—not only is there a bump, but also the surface of the road has become rough.
Buildup of these plaques causes three main problems:
Stiffening the blood vessel wall;
Narrowing the blood vessels; and
Increasing the likelihood of more plaque buildup.
High Blood Pressure

Regular stress can be a cause of high blood pressure.
Hypertension can be a result of many factors, including family history, genetics, stressors, personal tendency to be anxious or controlling (Type A qualities), diet, and more. Many of us might hear about elevated blood pressure from our physician as early as our mid-30s, so we start on a medication and forget about it. However, the medication only forces blood vessels to be open to reduce pressure; the pill doesn’t address the cause of why blood vessels were affected in the first place: plaque and the various factors that create plaque.
As we age, blood vessels can become stiff and inflexible because of natural wear and tear; however, the problem is also caused by plaque buildup from deposits of cholesterol and inflammation. The hardening of the arteries keeps the blood vessels from relaxing to help relieve blood pressure. In these cases, treatment is approached by helping to reduce the burden of plaque buildup as well as improving of mechanisms that breakdown plaque.
Although the big factors that seem out of our control are family history and genetics, it’s not true. In fact, having family history and genetics does not guarantee the development of disease. If this were true, every one of us would have all kinds of diseases that family members have had in the past. We learn from our family history about the risk factor and blind spots of which we must be aware. These include daily eating habits, exercising routines, health hygiene habits, and the ways of managing stress. With appropriate intervention, we can keep this “family history” from repeating and genetic weakness from expressing.
Treating Heart Disease
Ayurveda aids in the treatment of heart disease by helping us understand the cardiovascular system in an integrative way. Ayurveda is a different language and unique way of seeing things as whole systems. In looking at whole systems, we can treat whole systems. Our bodies through the lens of Ayurveda:
Metabolic function of the blood cells, hormones, and signals in circulation is controlled by the Ranjaka Pitta (an expression of the fire element);
Movement of heart muscle and blood vessels as well as movement of nutrition into and waste-product out of the tissues is controlled by Vyana Vayu (an expression of the air element); and
Nutrition from food that is carried in the plasma and immune cells are in-part governed by the Avalambaka Kapha. The plasma is the carrier of all the components of the bloodstream; it can separate from blood cells and flow into various tissues carrying nutrition and signals to all parts where blood can’t get.
Dietary Approach for Prevention
The DASH (Dietary Approach to Stop Hypertension) diet is a thoroughly researched way to help lower blood pressure and prevent heart disease. A systematic review of studies showed that this diet lowered blood pressure by several points and lowered total cholesterol and LDL cholesterol.3 In other words, this diet reduced components that contribute to plaque buildup as well as improved flexibility of the blood vessels to allow better adjustment to pressure.
Let us look at the daily components of this diet:4
6–8 servings of grains: one serving equals ½ cup of rice, pasta, cereal or 1 slice of bread. I recommend choosing low-glycemic grains like amaranth, quinoa, buckwheat, millet, wild rice, and brown rice.
4–5 servings of fruits: about two apples, pears, or oranges; ½ of a cantaloupe; ¼ of a watermelon; or a couple of handfuls of grapes or berries.
4–5 servings of vegetables: although recommendations of specific groups might change by underlying imbalance, a good mix of anti-inflammatory veggies and antioxidant-rich veggies are recommended.
6 servings of lean meat, poultry, or fish: these are useful sources of protein and all the enzymes, minerals, vitamins, and more associated with these proteins. They are useful, but not essential if you are vegetarian.
6 servings of lentils, nuts/seeds: I like to add seitan, tofu, and tempeh to this list as alternative vegetarian proteins.
2–3 servings of fat: as the Mayo Clinic describes, “Examples of one serving include 1 teaspoon soft margarine, 1 tablespoon mayonnaise, or 2 tablespoons salad dressing.” I don’t recommend any of these as your sources of fat. (See more about my fat recommendations below.)
I like to adapt this diet to our modern needs in a few ways. Depending on the individual and daily energy demand, I place an upper limit for grain intake and shift the caloric intake to add extra healthy fats. In a fresh-cooked meal, fats usually comes from what is added to that meal by the chef, except in case of diary or meats or eggs. So all the fat that we add can be used in a safe and digestible way to support the body’s structural and digestive needs. Also, fat has more caloric/energy output than carbs over time and is, in turn, better for sustaining energy over longer periods. Therefore, I encourage clients to have up to 3–4 teaspoons of raw coconut or olive/sesame oil every day, which is double the recommendation in the DASH diet. In doing so, patients make up for the calorie gap from cutting carbs while preventing blood sugar elevation that happens with eating a lot of carbs.
Healthy Muscles
Unique and different from other muscles of the body, the heart muscle is controlled by the nervous system with a well-regulated feedback mechanism. In turn, our heart muscle can become injured when it is forced to work too hard, is exposed to unhealthy foods, or becomes weakened due to a clot or bleed (aka a heart attack).
High blood pressure causes the heart muscle to work harder against the resistance of the blood vessels to push blood out to all the extremities of the body. This could cause the heart muscle to grow thicker, much like other muscles of the body grow bigger when they are used.
But, unlike all other muscles, when heart grows, it doesn’t have much room to spread out. Also, the space inside the heart, where blood is filled before being pumped, becomes narrower. The result is that the heart becomes less efficient at pumping an adequate amount of blood with each pulse.5
In addition, an unhealthy diet can worsen the problem by reducing the quality of the heart muscle and, in turn, weakening the contraction strength of the heart. The risk of clots and bleeds in the heart muscle increases as plaques in the arteries become thicker and less stable.
The heart muscle can be protected by reducing the unnecessary stress on the heart by treating blood pressure at the root cause. The quality of the heart muscle can be improved with better diet that reduces oxidative damage and promotes efficient repair of the heart muscle. Diet also provides the basic building blocks and supportive structural and functional factors that make a healthy heart.6
Another way is to stimulate the heart muscle in the right way is to become more efficient. For this, we perform aerobic cardio exercises, like hiking, swimming, cycling, elliptical, brisk walking, interval training, and more.
In conclusion, proper maintenance of the heart is a very dynamic process. The internal environment, the cardiovascular system, is very responsive to the outer environment of the person. The heart responds to every physical and emotional experience of a person. It’s also highly responsive to what a person eats, drinks, or breathes. This teaches us that daily unhealthy exposures in the form physical and emotional stress, unhealthy diet and lifestyle, and more, lead to heart disease; therefore, health-promoting steps must be taken as part of our daily routines.
The heart’s health is intricately dependent on the health of the arterial system. Prevention of plaque build-up in the arteries and lowering high blood pressure are primary ways to reduce cardiovascular risk. Additionally, we can strengthen the heart muscle with individualized dietary recommendations and exercise stimulation.
References
1.CDC.gov. Centers for Disease Control and Prevention. “Million Hearts: strategies to reduce the prevalence of leading cardiovascular disease risk factors.” United States, 2011. MMWR. 2011;60(36):1248–51.2.Heart.org. American Heart Association. “Atherosclerosis.” Last updated: April, 21, 2014; accessed October 16, 2016.3.Siervo M, et al. “Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis.” Br J Nutr. 2015 Jan 14;113(1):1-15.4.MayoClinic.org. The Mayo Clinic. “DASH diet: Healthy eating to lower your blood pressure.” April 8, 2016. Online article accessed October 16, 2016.5.Figeroa MS, et al. “Congestive Heart Failure: Diagnosis, Pathophysiology, Therapy, and Implications for Respiratory Care” Respir Care. 2006;51(4):403–412.6.Rothberg MB and Sivalingam SK. “The New Heart Failure Diet: Less Salt Restriction, More Micronutrients.” J Gen Intern Med. 2010 Oct; 25(10): 1136–1137.




